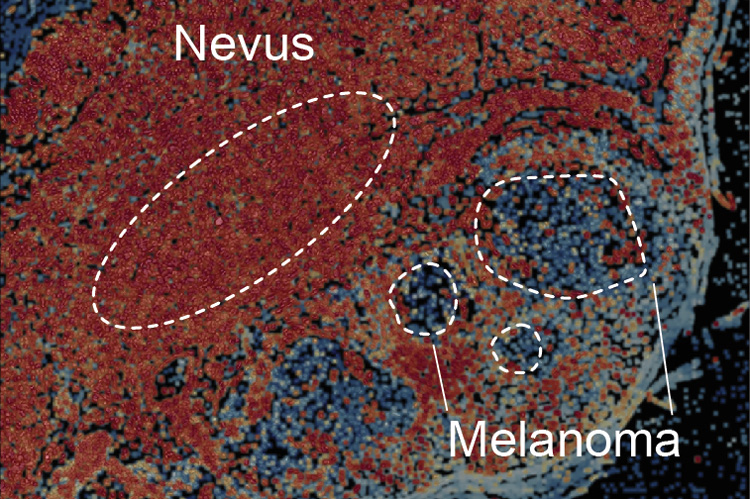
This skin section shows a benign mole or nevus that is transitioning into a melanoma, the most serious type of skin cancer. New experiments by UC Berkeley and UCSF researchers suggest that immortalization of skin cells, which is essential to turning them cancerous, is a two-step process: a mutation in nevus cells slightly raises levels of telomerase, which keep the cells alive long enough for a second change, still unknown, that up-regulates telomerase to make the cells immortal and malignant. (Credit: Image by Dirk Hockemeyer/UC Berkeley and Boris Bastian/UCSF)
—————————————————————————————————————————————–
Covid-19, Coronavirus updates
———————————————————————————————————————————-
Find jobs in R & D, Medicine, engineering and a wide variety of scientific fields and others in our jobs page.
—————————————————————————————————————————————–
Explore resources for science students engaged in life science courses and other scientific fields with practice tests, mcqs at our Student Zone.
———————————————————————————————————————
A mutation that helps make cells immortal is critical to the development of a tumor, but new research at UC Berkeley suggests that becoming immortal is a more complicated process than originally thought.
The key to immortalization is an enzyme called telomerase, which keeps chromosomes healthy in cells that divide frequently. The enzyme lengthens the caps, or telomeres, on the ends of chromosomes, which wear off during each cell division.
When the telomeres get too short, the ends stick to one another, wreaking havoc when the cell divides and in most cases killing the cell. The discovery of telomerase and its role in replenishing the caps on the ends of the chromosomes, made by Elizabeth Blackburn and Carol Greider at UC Berkeley and John Szostak at Harvard University in the 1980s, earned them a Nobel Prize in Physiology or Medicine in 2009.
Because telomeres get shorter as cells age, scientists theorized that cancer cells – which never age – become immortalized by turning on production of telomerase in cells that normally don’t produce it, allowing these cells to keep their long telomeres indefinitely. An estimated 90 percent of all malignant tumors use telomerase to achieve immortality, and various proposed cancer therapies focus on turning down the production of telomerase in tumors.
The new research, which studied the immortalization process using genome-engineered cells in culture and also tracked skin cells as they progressed from a mole into a malignant melanoma, suggests that telomerase plays a more complex role in cancer.
“Our findings have implications for how to think about the earliest processes that drive cancer and telomerase as a therapeutic target. It also means that the role of telomere biology at a very early step of cancer development is vastly under-appreciated,” said senior author Dirk Hockemeyer, a UC Berkeley assistant professor of molecular and cell biology. “It is very likely that what we find in melanoma is true for other cancer types as well, which would warrant that people look more carefully at the role of early telomere shortening as a tumor-suppressing mechanism for cancer.”
The results were reported online August 17 as a “first release” publication from the journal Science.
From nevus to cancer
Hockemeyer and his UC Berkeley colleagues, in collaboration with dermatopathologist Boris Bastian and his colleagues at UCSF, found that immortalization is a two-step process, driven initially by a mutation that turns telomerase on, but at a very low level. That mutation is in a promoter, a region upstream of the telomerase gene – referred to as TERT – that regulates how much telomerase is produced. Four years ago, researchers reported that some 70 percent of malignant melanomas have this identical mutation in the TERT promoter.
The TERT promoter mutation does not generate enough telomerase to immortalize the pre-cancerous cells, but does delay normal cellular aging, Hockemeyer said, allowing more time for additional changes that turn telomerase up. He suspects that the telomerase levels are sufficient to lengthen the shortest telomeres, but not to keep them all long and healthy.
If cells fail to turn up telomerase, they also fail to immortalize, and eventually die from short telomeres because chromosomes stick together and then shatter when the cell divides. Cells with the TERT promoter mutation are more likely to up-regulate telomerase, which allows them to continue to grow despite very short telomeres. The marginal levels of telomerase in the cell, Hockemeyer said, result is some unprotected chromosome ends in the surviving mutant cells, which could cause mutations and further fuel tumor formation.
“Before our paper, people could have assumed that the acquisition of just this one mutation in the TERT promoter was sufficient to immortalize a cell; that any time when that happens, the telomere shortening is taken out of the equation,” Hockemeyer said. “We are showing that the TERT promoter mutation is not immediately sufficient to stop telomeres from shortening.”
It is still unclear, however, what causes the eventual up-regulation of telomerase that immortalizes the cell. Hockemeyer says that it’s unlikely to be another mutation, but rather an epigenetic change that affects expression of the telomerase gene, or a change in the expression of a transcription factor or other regulatory proteins that bind to the promoter upstream of the telomerase gene.
“Nevertheless, we have evidence that the second step has to happen, and that the second step is initiated by or is occurring at a time when telomeres are critically short and when telomeres can be dysfunctional and drive genomic instability,” he said.
In retrospect, not a surprise
Though most cancers seem to require telomerase to become immortal, only some 10 to 20 percent of cancers are known to have a single-nucleotide change in the promoter upstream of the telomerase gene. However, these include about 70 percent of all melanomas and 50 percent of all liver and bladder cancers.
Hockemeyer said that the evidence supporting the theory that the TERT promoter mutation up-regulated telomerase has always been conflicting: Cancer cells tend to have chromosomes with short telomeres, yet have higher levels of telomerase, which should produce longer telomeres.
According to the new theory, the telomeres are short in precancerous cells because telomerase is turned on just enough to maintain but not lengthen the telomeres.
“Our paper reconciles contradictory information about the cancers that carry these mutations,” Hockemeyer said.
The finding also resolves another recent counterintuitive finding: that people with shorter telomeres are more resistant to melanoma. The reason, he said, is that if a TERT promoter mutation arises to push a precancerous lesion – the mole or nevus – toward a melanoma, the chances are greater in someone with short telomeres that the cell will die before it up-regulates telomerase and immortalizes the cells.
The study also involved engineering TERT promoter mutations in cells differentiated from human pluripotent stem cells and following their progression toward cellular immortality. The results were identical to the progression seen in human skin lesions obtained from patients in UCSF’s Helen Diller Family Comprehensive Cancer Center and examined in the Clinical Cancer Genomics Laboratory, which Bastian directs.
Source: University of California – Berkeley.
Published on 5th September 2017


